
The PEGASUS Equity Project is an extension of the PEGASUS ARGENTINA Program, an implementation science-based program designed to improve pediatric TBI outcomes through improved guideline adherence and is currently being carried out in South America. PEGASUS Equity which is based in the United States, is focused on expanding this work by identifying ways to improve equitable practices and reduce racial and ethnic disparities at Level I and Level II Trauma Centers in the US. This study has received institutional review board approval [UW IRB: STUDY00016161].
Short- and long-term health outcomes of pediatric TBI are worse for populations based upon geographic location and racial/ethnic identity. To identify barriers and facilitators to equitable care, healthcare providers and administrators at Level I and Level II Trauma Centers will share their expertise and engage in conversations through a survey, focus group, or interview.
Below are the aims for our research study:
Specific Aim 1: Characterize racial/ethnic disparities in acute pediatric TBI care in the U.S. We will use the National Trauma Databank to describe guideline adherence (intracranial pressure monitoring rate, timing, and duration) by racial/ethnic patient groups across facility types. We will cluster ICP monitoring outcomes by trauma center designation both within and across centers.
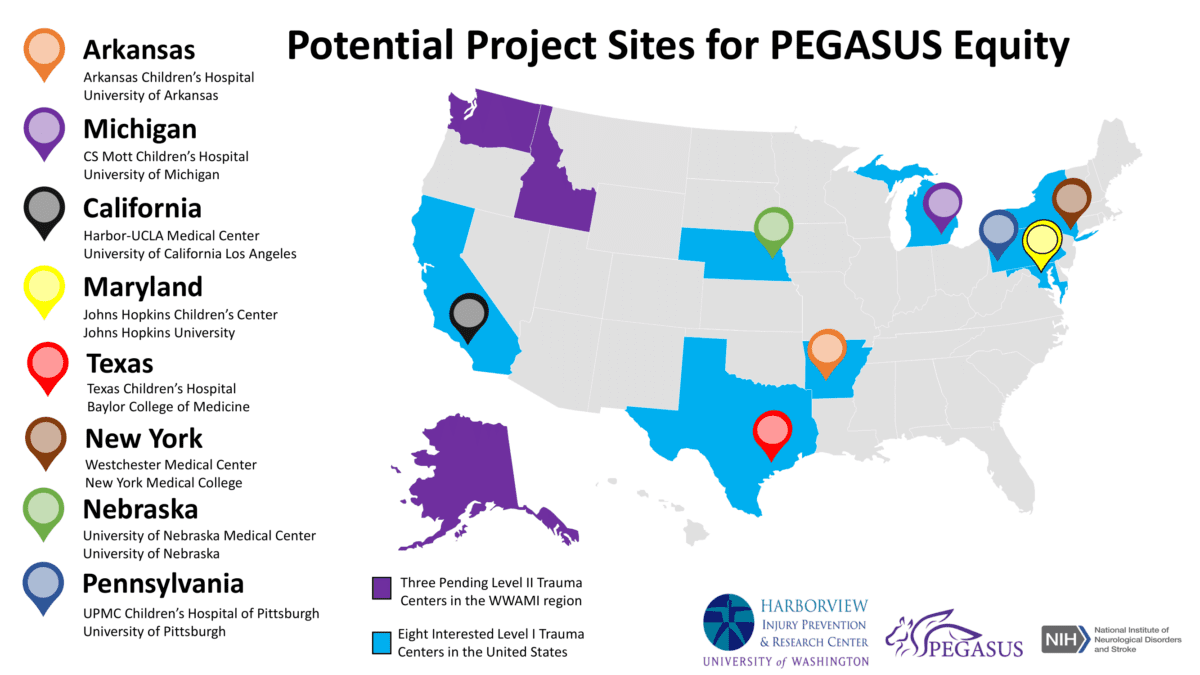
Specific Aim 2: Identify barriers and facilitators to achieving equity in acute pediatric TBI care in the U.S. Through survey procedures, interviews, and focus groups, we will identify barriers and facilitators to equitable TBI guideline adherence by Level I and Level II trauma centers. Through community engaged approaches, participating trauma centers will identify strategies to achieving equity in acute TBI care processes, which we well assess by facility characteristics, geographic location, and populations served.
An expected outcome of the proposed research is the development of an equity assessment tool that we anticipate incorporating into the PEGASUS program to improve equitable implementation of acute pediatric TBI care in the U.S. Through this work, we will develop a network of level I and II pediatric trauma centers who will be potential adopters of the equity assessment tool either as a stand-alone or as part of the PEGASUS program.
Harborview Injury Prevention & Research Center at the University of Washington
Funded by the NIH – National Institute of Neurological Disorders and Stroke
Monica Vavilala, MD is a Professor of Anesthesiology and Pain Medicine at the University of Washington and a clinically active anesthesiologist at Harborview Medical Center. She directs the UW Harborview Injury Prevention and Research Center, leads the TBI section, and co-directs the UW Pediatric Injury Research T-32 Training. Dr. Vavilala has over 20 years of experience focusing on prevention and improving TBI outcomes and has translated research on basic mechanisms of physiologic and inflammatory response to injury into successful clinical trials and ultimately into the development of international evidence-based clinical practice guidelines and changes in health policy.
Chelsea Hicks is a NIH T32 Post-Doctoral Fellow in the Pediatric Injury Research Training Program at UW Harborview Injury Prevention and Research Center. She received her PhD and MPH in Occupational and Environmental Health with a specialty in Injury and Violence Prevention. She has a background in biology and community engagement, and has obtained training in interviewing methods through hospital readmission and injury prevention work as a research assistant at Massachusetts General Hospital. Dr. Hicks also served as a Research Fellow for the Division of Violence Prevention at the CDC with the Violence Against Children Survey (VACS) Team, and her prior research involves pediatric violence prevention and violence trends in communities impacted by natural hazardous events.
Dr. Theresa Hoeft is a Research Assistant Professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington. She is a mental health services researcher with an interest in improving access to mental health care, in particular for those with unmet social needs. Dr. Hoeft has a background in population health with specific training in health economics, health services research, mixed-methods research, and community-based participatory research (CBPR), and is an expert in interdisciplinary collaborations which engage diverse partners toward improving population health.
Dr. Bryan Weiner is a Professor in the Departments of Global Health and Health Systems & Population Health at the University of Washington. He is an organizational psychologist by training, and his research focuses on the adoption, implementation, and sustainment of innovations and evidence-based practices in health care organizations. Dr. Weiner currently serves as PI of a newly funded research center to develop and refine novel methods for optimizing the implementation of evidence-based interventions in cancer control, and he also collaborates in a wide-range of research efforts to implement and scale-up evidence-based interventions in low- and middle-income countries including maternal and child health, mental health, hypertension, TBI, and HIV interventions.
Pediatric traumatic brain injury (TBI) is a leading cause of death and disability in the U.S. and worldwide. Disparities in acute adult TBI care are observed, recognized, and are reported but such data in pediatric TBI are limited. However, short- and long-term health effects of pediatric TBI are worse for populations based upon geographic location and identifying as racial/ethnic minorities. Structural barriers to acute TBI care such as large acute care medical expenditures, lack of access to educational support mechanisms for caregivers, and comorbidities such as mental health complications badly affect patients and families. Children injured in rural locations have more than twice the odds of mortality than pediatric injuries treated at urban centers, but acute TBI care was not examined in these studies. Another study showed that African American, Hispanic, and Native American communities experienced longer hospital length of stay, and girls had higher medical complications related to TBI injuries than boys.
For more information on TBI or the PEGASUS Argentina Project, visit our PEGASUS homepage.