
Workplace violence in healthcare has continued to grow throughout the years. Inside hospital’s emergency departments there are frequent assaults against healthcare workers.
Researchers at the Harborview Injury Prevention & Research Center (HIPRC), UW Medicine, the Department of Emergency Medicine of the University of Washington School of Medicine, Yale School of Medicine, and the University of Washington’s School of Social Work have conducted a new study that identifies a framework for addressing workplace violence in the emergency department’s (ED). This study was published Friday, December 4, 2020 in the Journal of Occupational and Environmental Medicine.
Researchers interviewed ED staff at five different sites across the U.S. Two of the sites were located in a healthcare system in the Northeast with Ambrose H. Wong, MD, MSEd leading that work and three located in a healthcare system in the Pacific Northwest lead by Marie C. Vrablik MD, MCR, HIPRC associate member . “Using data from victim’s experiences across two geographically different institutions, we were able to identify concepts and themes that established the framework developed in this study,” says lead researcher Marie C. Vrablik.
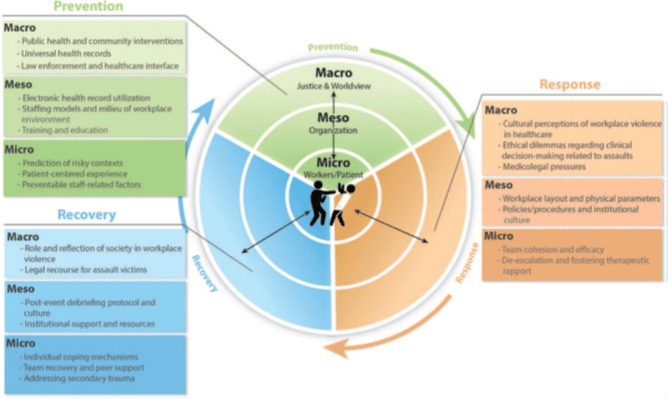
Strategies to address violence in the workplace were provided at the “macro, meso, micro” levels and included a focus on “prevention, response, recovery.”
By using this framework Vrablik says hospitals and healthcare systems can work to prevent and better respond to violence in the ED.
“Our results suggest that using a socioecological framework to understand staff experiences of workplace violence can lead to a more comprehensive approach to prevention and response in the future. Hospitals and EDs can use our findings to help guide their prevention, recovery and response efforts for workplace violence.” says Megan Moore, PhD MSW, Co-Director of HIPRC outreach core, and Associate Director of HIPRC’s research core.
Examples of strategies identified by participants include the importance of identifying risky contexts and environments, training on de-escalation techniques, providing a patient-centered experience, effective staffing models, team and peer support, and debriefing.
Funding for this study was received from institutional board approval from Yale University and University of Washington and followed the 32-item consolidated criteria for reporting qualitative research (COREQ). Dr. Vrablik was funded by the State of Washington Department of Labor & Industries Safety and Health Investment Projects Program. Dr. Wong is supported by the Robert E. Leet and Clara Guthrie Patterson Trust Mentored Research Award and the KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health and the National Institutes of Health Roadmap for Medical Research.
Some of the researchers in this study are part of HIPRC’s Injury-related Health Equity Across the Lifespan (iHeal). The group’s mission is to work with multidisciplinary researchers, medical providers, and community stakeholders to identify and address disparities in injury-related healthcare. iHeal is committed to creating a respectful workspace together as they seek to identify and correct structural biases that perpetuate inequities in health and well-being. iHeal aims to dismantle biases based on age, disability, ethnicity, indigenous group membership, gender identity, linguistic differences, national origin, race, religion, sexual orientation, and social class.